Background: Osteoporosis is commonly found in thalassemia patients; however, its pathogenesis is not thoroughly understood. Metabolomics is the study of metabolites in biofluids, which help to elucidate the underlying mechanism of several metabolic diseases. Nevertheless, plasma metabolomics profiling has not been carefully investigated in thalassemia patients with low bone mineral density (BMD).
Objective: To investigate the alterations of plasma targeted metabolomics in adult thalassemia patients with low BMD.
Methods: We conducted a cross-sectional study from February 2022 to January 2023 at Outpatient Hematology Clinic, Chiang Mai University. Thalassemia patients, confirmed by HPLC hemoglobin typing, who aged 19-50 years (male) or more than 19 years (premenopausal female) were eligible. Exclusion criteria were (1) current use or history of any bone modifying agent use within 1 year, (2) severe hepatic or renal impairment, (3) active malignancy or infection. Age- and sex-matched with normal body mass index were also recruited as controls. Two-point BMD, plasma targeted metabolomics by using liquid chromatography coupled with mass spectrometry (LC/MS), and serum bone turnover markers, including bone resorption using CTX, and bone formation using P1NP, were assessed. Interested metabolomes included 19 amino acids, 7 free fatty acids, 20 acylcarnitine intermediates of branched-chain amino acids and fatty acids, 37 phospholipid derivatives, and 4 Krebs' cycle metabolomes. Low BMD was defined as a Z-score of less than -2.0 at any site. Outcomes were the alterations of plasma levels of metabolomes among control, thalassemia with normal BMD, and thalassemia with low BMD.
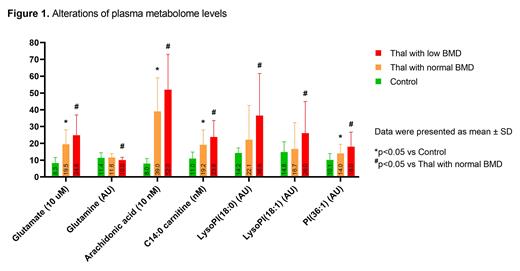
Results: There were a total of 80 thalassemia patients and 40 controls recruited. The mean age of patients was 34.8 years (SD 8.7). Twenty-six patients (32.5%) were male. Forty-seven patients (58.8%) were transfusion-dependent thalassemia. Low BMD was detected in 37 patients (47.5%). We found several plasma metabolomes that were significantly changed between controls and thalassemia and further altered when compared between thalassemia with normal BMD and low BMD (Figure 1). Considering plasma amino acids, glutamate level was significantly increased while glutamine level was decreased. Regarding fatty acid-related metabolomes, arachidonic acid level was increased in thalassemia with low BMD. In addition, several fatty acid-derived medium- and long-chain acylcarnitine levels were higher in plasma of thalassemia with low BMD, particularly C14:0 carnitine. Among plasma phospholipid derivatives, phosphatidylinositol (PI) and lysoPI levels were significantly increased in thalassemia with low BMD. Four plasma Krebs' cycle metabolites were not different among groups. Surprisingly, two serum bone turnover markers (CTX and P1NP) were not sensitive for detecting low bone mineral density in thalassemia (Control vs Thalassemia with normal BMD vs Thalassemia with low BMD: CTX 0.27±0.17 vs 0.36±0.20 vs 0.34±0.19 ng/mL, p=0.079 and P1NP 57.2±25.0 vs 57.2±34.0 vs 53.7±26.4 ng/mL, p=0.824).
Conclusion: There were several changes in plasma metabolome levels among thalassemia with low BMD, including altered glutamate-glutamine metabolism, impaired fatty acid oxidation, and increased plasma phosphatidylinositol. Interestingly, these changes were found in patients with normal BMD and further increased in patients with low BMD. Our findings suggest the role of plasma metabolomics as non-invasive biomarkers for osteoporotic condition in thalassemia patients.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal